Cardiologists are welcoming the arrival of a new device-based hypertension treatment called renal denervation and asking Medicare to cover the procedure for a large patient population.
Doctors, medical groups and others have endorsed national reimbursement for renal denervation in dozens of public comments submitted to the Centers for Medicare and Medicaid Services ahead of a final Medicare coverage decision expected by early October. Many cite concern about the high numbers of patients whose blood pressure remains poorly controlled despite the availability of multiple drug treatments.
Roughly three-quarters of U.S. adults with hypertension do not have it under control. Writing in favor of the national coverage determination, or NCD, physicians recounted seeing first-hand the consequences of uncontrolled blood pressure in patients who suffered stroke, heart attack, heart failure and kidney disease. The doctors view renal denervation as a much-needed option to stop the progression.
“Renal denervation (RDN) represents a significant breakthrough, providing a novel tool to lower blood pressure and reshape long-term outcomes in ways that once seemed out of reach,” Oluwaseun Akinseye, an interventional cardiologist at Methodist Le Bonheur Healthcare in Memphis, Tennessee, said in comments to the CMS.
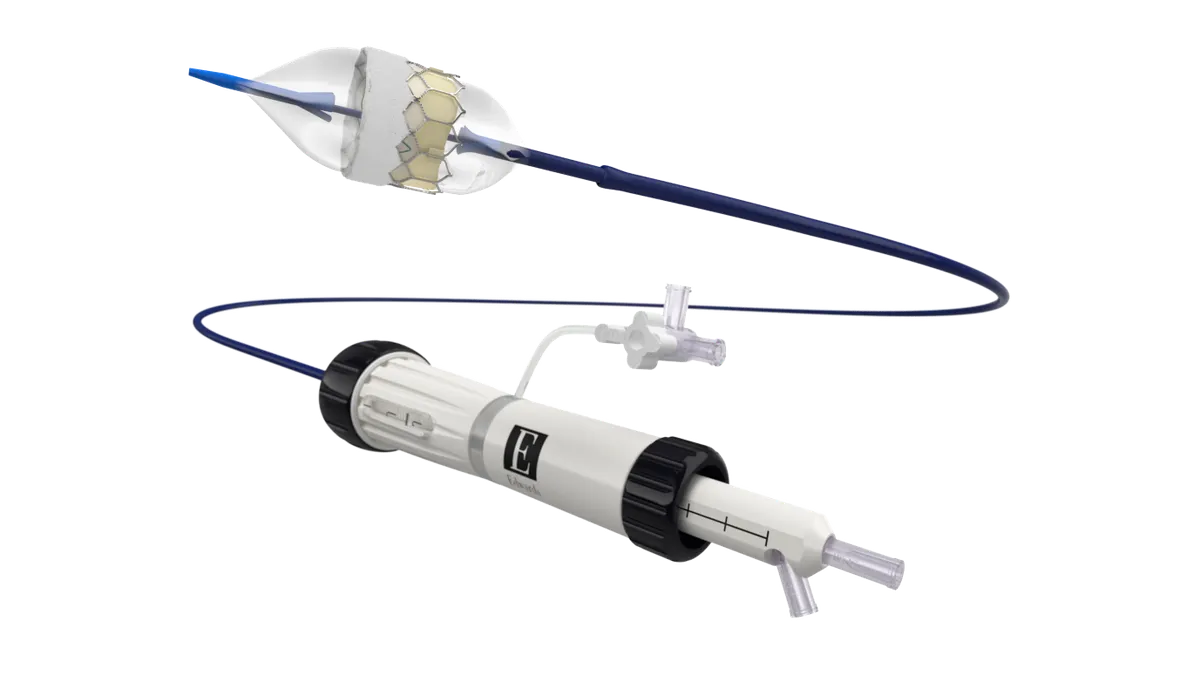
In late 2023, the Food and Drug Administration approved two renal denervation devices: Medtronic’s radiofrequency-based Symplicity Spyral and Recor Medical's ultrasound-based Paradise system. Limited insurance reimbursement, however, has slowed clinical adoption.
The CMS NCD is expected to accelerate use of the minimally invasive procedure for patients whose blood pressure hasn’t improved despite lifestyle changes and medications.
In their comments to the CMS, numerous cardiologists described positive early experiences with the procedure.
Eric Secemsky, of Beth Israel Deaconess Medical Center and Harvard Medical School, said all of the more than 30 patients treated with renal denervation in his multidisciplinary hypertension program were discharged the same day without procedural complications and had sustained blood pressure improvement.
“Our only significant barrier to date has been the lack of reimbursement,” Secemsky told the CMS.
Omar Hyder, from the Brown University Health Cardiovascular Institute, described the treatment as safe, straightforward and extremely effective, after performing just over 20 procedures. “In a subset of patients,” he noted, “we have seen even more drastic reductions in blood pressure requiring the weaning of medications.”
The long road to approval
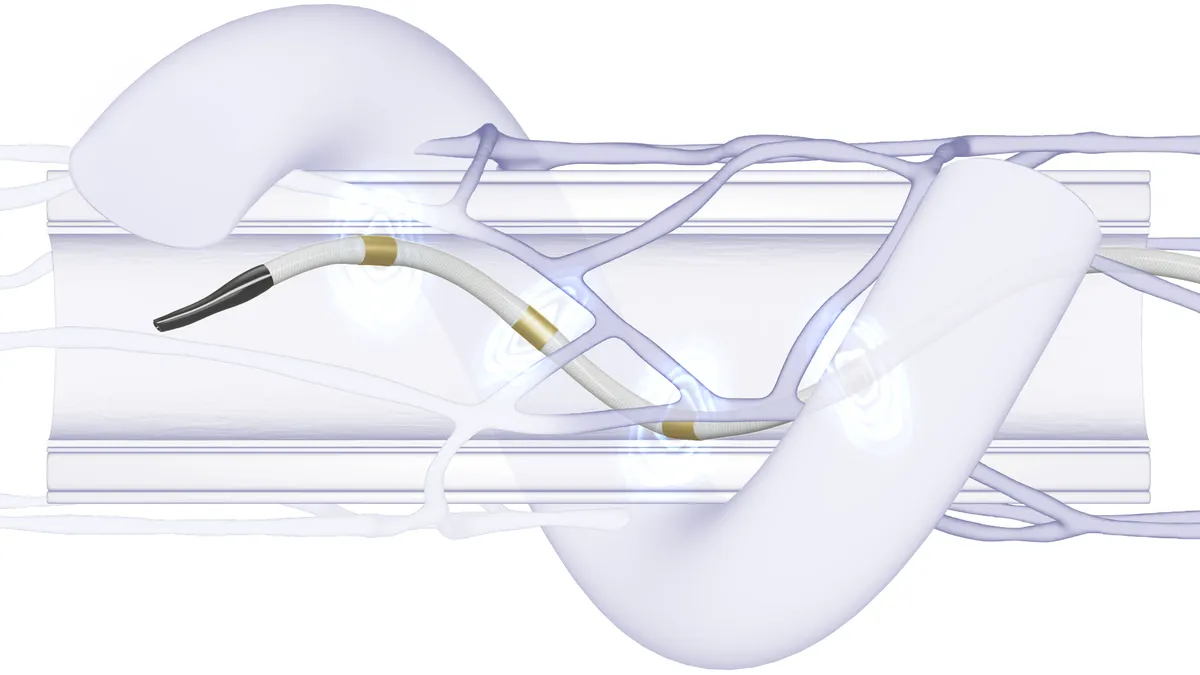
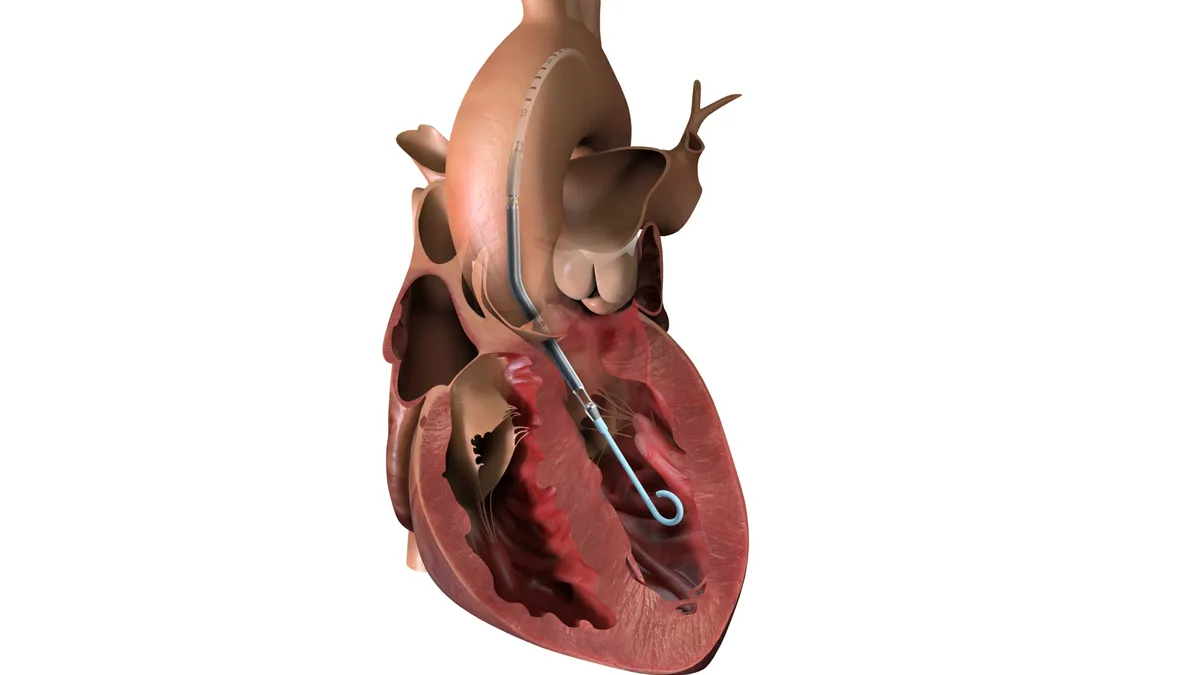
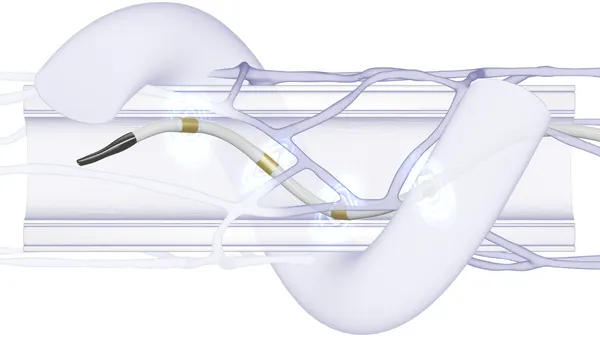
During a renal denervation procedure, energy doses are sent to ablate overactive nerves near the kidneys that contribute to high blood pressure. The reduced nerve activity causes a drop in blood pressure.
While physician interest in the technology is growing, its potential for success was not always clear.
Medtronic’s work on renal denervation picked up steam with the 2011 purchase of Ardian, developer of the Symplicity catheter. Along the path to FDA approval, the treatment faced research setbacks that triggered considerable debate about its effectiveness.
A major obstacle emerged in 2014, when the SYMPLICITY HTN-3 pivotal trial failed to meet its efficacy endpoints. Although the procedure proved safe, the study found no significant difference in blood pressure reduction between the treatment and sham groups.
Medtronic pushed on with redesigned studies. However, in 2022, another trial, the SPYRAL HTN-ON MED study, missed its primary efficacy endpoint. The result contributed to an FDA advisory panel’s negative benefit-risk assessment before the agency ultimately approved Medtronic’s device. Patients not taking antihypertensive medications, evaluated in the pivotal SPYRAL HTN-OFF MED trial, had statistically significant blood pressure reductions, and that study met its effectiveness endpoint.
The proposed NCD, along with new hypertension treatment guidelines from the American College of Cardiology and American Heart Association, validates renal denervation as an additional option for managing hypertension in patients who do not sufficiently respond to lifestyle modifications and pharmaceutical treatments, a Medtronic spokesperson said in an email.
“The proposed NCD represents a novel, meaningful market for Medtronic,” the spokesperson said. "To date, we are seeing great interest from healthcare systems across the United States that are looking to offer the Symplicity blood pressure procedure."
Recor’s pivotal study met its primary safety and effectiveness goals, and the FDA approved the Paradise device after a positive panel vote.
Both ablation methods — ultrasound and radiofrequency — won FDA authorization despite demonstrating only modest reductions in absolute blood pressure values in their phase 3 clinical trials, said Stanford University School of Medicine’s Vivek Bhalla. But the data are noteworthy, he wrote, because “even a modest reduction has a substantial effect on lowering cardiovascular risk.”
Furthermore, subsequent registry data point to a sustained drop in blood pressure over time, wrote Bhalla and other doctors.
“Reimbursement for these procedures is a necessary step to translate these research studies to the broader public to improve the woefully poor rates of blood pressure control in the United States,” Bhalla told the CMS.
Real-world care
Michael Rosenberg, who has performed about 30 renal denervation cases over the past year using Recor’s device, said the research to date has not told the whole story.
“Results have been better than the literature has suggested and patient satisfaction has been very high. I would say it has been a resounding success from the standpoint of patient welfare, outcome, and safety,” said Rosenberg, an interventional cardiologist at Froedtert South Medical Center in Kenosha, Wisconsin.
A recurring theme from supporters of the procedure centered on how high blood pressure should be defined, with many arguing the CMS’ proposed threshold of 140/90 mm Hg is too restrictive.
In comments to the CMS on the NCD, the ACC, Society of Cardiovascular Angiography & Interventions, and Society for Vascular Medicine jointly recommended the agency adopt a definition based on systolic blood pressure greater than 140 mm Hg, without a diastolic requirement, to avoid excluding patients with isolated systolic hypertension, which is common in older adults.
The groups, along with many doctors, also urged greater flexibility in requirements for medication timelines, doctor visits, and multidisciplinary hypertension screening and treatment programs.
Araya Negash, an interventional cardiologist at Corewell Health in Grand Rapids, Michigan, cautioned against adopting policies that could inadvertently limit treatment only to those with the means to seek out specialized services.
“As we enter a new era” in hypertension management, wrote Negash, “it is essential that we balance innovation with equitable access to ensure that all patients who could benefit from this therapy are able to receive it.”