Dive Brief:
-
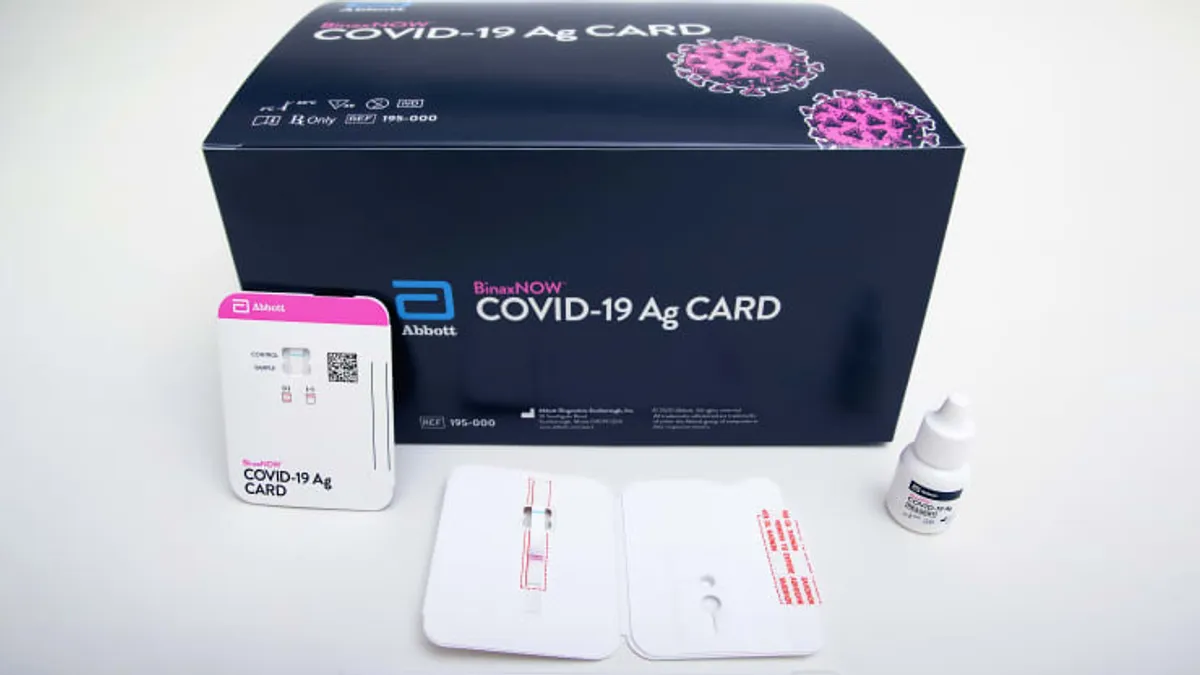
Abbott's rapid point-of-care BinaxNOW antigen test may miss nearly two-thirds of COVID-19 infections in people without symptoms, according to a new CDC study.
-
The researchers used BinaxNOW and PCR to analyze 3,419 paired specimens collected at two community testing sites in Pima County, Arizona, which includes Tucson. Compared to PCR, BinaxNOW had a 35.8% sensitivity when used to analyze samples taken from asymptomatic individuals.
- However, the study also generated evidence that BinaxNOW catches most infectious cases. In a subset of asymptomatic patients likely to be infectious, the sensitivity was 78.6%. Abbott said in a written response to the study that BinaxNOW is "great at finding infectious people."
Dive Insight:
The fast turnaround times and low cost of antigen tests makes them attractive to schools and other institutions seeking to prevent coronavirus transmission. By frequently testing everyone who enters a site, it may be possible to find the pre-symptomatic or asymptomatic individuals estimated to cause 50% of COVID-19 transmission.
However, the inferior sensitivity of antigen tests means they miss more cases than PCR, leading some experts to argue against their use in mass screening programs.
To better understand how BinaxNOW, a $5, instrument-free test, performs in the real world, CDC had two community COVID-19 testing centers in Arizona take two samples from 3,419 people. Taking two samples from each individual enabled the agency to compare the performance of BinaxNOW to PCR.
Compared to PCR, BinaxNOW had a sensitivity of 35.8% in asymptomatic people, rising to 64.2% in people with COVID-19 symptoms. The finding suggests BinaxNOW misses a significant number of positive cases.
Yet, the impact of those false negatives on efforts to control the virus may be less significant than the top-line findings suggest. CDC attempted to culture most samples that tested positive on either test. As positive viral culture indicates the presence of infectious virus, the process enabled CDC to assess if BinaxNOW is identifying the individuals most likely to transmit the pathogen.
In the asymptomatic, viral culture positive subpopulation, BinaxNOW had a sensitivity of 78.6%. The sensitivity rose to 92.6% in symptomatic people with positive viral culture results. The researchers said the finding "might reflect better performance for detecting infection in a person with infectious virus present."
Specificity was near-100% in the overall population, suggesting BinaxNOW very rarely delivers a false positive. The finding is in line with expectations, although FDA did issue a notice in November about the potential for false positives when using such antigen tests.
At the time, FDA said it was aware of reports of false positive results associated with antigen tests used in nursing homes and other settings. The agency emphasized that antigen tests are "indicated for the qualitative detection of SARS-CoV-2 antigens in authorized specimen types collected from individuals who are suspected of COVID-19 by their healthcare provider within a certain number of days of symptom onset."
FDA also noted that antigen tests are not as sensitive as molecular tests and reminded clinical laboratory staff and healthcare providers that negative results from an antigen test may need to be confirmed with a molecular diagnostic prior to making treatment decisions.
The CDC study adds to a body of evidence on the use of antigen tests, some of which have delivered divergent results. A similar comparison of BinaxNOW and PCR in a community screening program found Abbott's test had an overall sensitivity of 89.0%. BD previously found its antigen test achieved a similar sensitivity to PCR, although that study analyzed a smaller number of samples collected from multiple sites.
Still, Abbott contends that having a rapid antigen test like the 15-minute BinaxNOW diagnostic "gives the patient critical information at a point in the infection cycle when they're at the highest risk of spreading disease, making it a powerful tool in preventing transmission compared to a 24-hour turnaround PCR test."