Dive Brief:
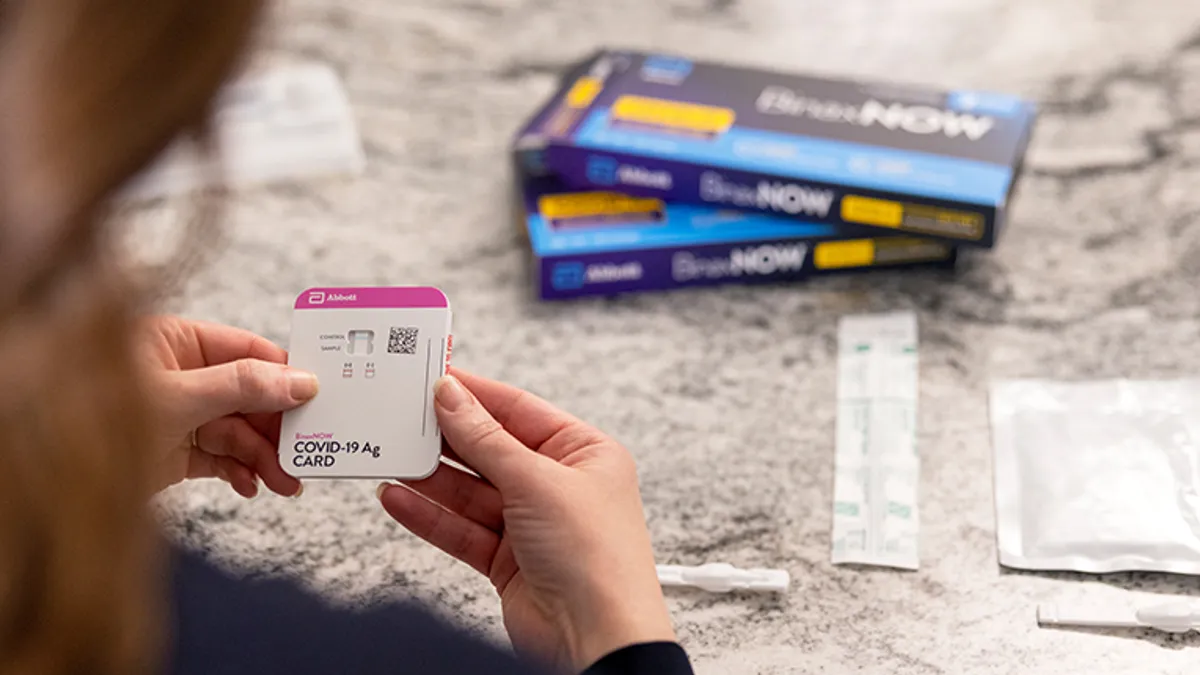
- Abbott Laboratories' BinaxNOW and Quidel's QuickVue rapid antigen tests may fail to detect the COVID-19 omicron variant during the early infectious period, according to a small real-world study that has yet to be peer reviewed.
- The preprint study, posted online Wednesday, looked at samples taken during routine workplace coronavirus surveillance testing. The median time from first positive PCR to first antigen test positive was three days. During the false negative period, four of the 30 people in the cohort are known to have transmitted the virus. Based on the findings, members of the COVID-19 Sports and Society Working Group behind the study questioned the use of current nasal swab rapid antigen tests in workplace screening.
- An Abbott spokesperson in an emailed statement acknowledged that "PCR tests are more sensitive than antigen tests — this is not new information" adding "our studies confirm that BinaxNOW continues to detect the omicron variant at comparable viral load levels as all other variants and the original SARS-CoV-2 strain." A Quidel spokesperson declined to comment on the study, instead referring to the company's Dec. 28 statement claiming that its antigen tests "continue to detect COVID-19 variants such as omicron."
Dive Insight:
FDA flagged up a potential problem with the use of antigen tests to detect omicron infections late last year. In early testing using patient samples containing live virus, the agency found antigen tests may have lower sensitivity against omicron than earlier variants. The new preprint study adds to the concerns and puts forward ideas for why omicron may cause more false negatives.
To assess the impact of omicron on antigen tests, the researchers looked at results from five workplaces in New York, Los Angeles and San Francisco that suffered omicron outbreaks. The researchers limited their focus to people who were taking daily tests at the time of diagnosis and had paired saliva PCR and nasal antigen test results from around the day they first provided a positive sample.
Targeting the cohort of 30 cases enabled the researchers to assess if there was lag between PCR and antigen test positivity. What they found was that the median lag between the first positive PCR and antigen test results was three days. False negatives were delivered by both Abbott BinaxNOW and Quidel QuickVue, the only two rapid antigen tests used in the study.
On one level, the discovery of a lag is unsurprising. PCR tests are known to be more sensitive and therefore more able to detect low levels of virus early in an infection. The question is whether the cases were a risk to others at the time of the false negatives or if they only became infectious later.
Based on analysis of PCR cycle thresholds for the positive samples, the researchers calculate 28 of the 30 people had viral loads within the range of confirmed omicron transmissions. Four of the people passed on the virus when the antigen tests gave negative results.
An analysis of samples from a subgroup of five people offers a potential explanation for the lag. Testing showed viral load in saliva peaked one to two days earlier than the nasal samples. The finding is in line with another preprint publication that found saliva is the preferred sample for detecting omicron, which appears to infect the bronchus faster than delta.
The Abbott spokesperson's emailed statement cites another recent preprint study from Brigham and Women's Hospital and Harvard that the company contends showed strong performance of its BinaxNOW antigen test.
"We are confident in BinaxNOW's ability to detect people who are infectious, including those with the omicron variant," the spokesman said.
Greg Slabodkin contributed reporting.