Dive Brief:
-
A trade group representing laboratories including LabCorp and Quest Diagnostics has asked President Joe Biden to make more money available to test uninsured people for COVID-19.
-
The federal government is currently supporting the testing of uninsured people through a $2 billion fund. Yet, the fund is almost depleted, leading the American Clinical Laboratory Association to write to Biden to request more money.
-
ACLA also said its members have seen health plans deny more than 1 million COVID-19 PCR tests since June and coverage uncertainty has created barriers for accessing diagnostics. The trade group wants Biden to close "testing coverage loopholes" to ensure access to COVID-19 diagnostics. America’s Health Insurance Plans (AHIP), whose members include major healthcare insurers, was not immediately available for comment, though it has accused out-of-network labs of price gouging.
Dive Insight:
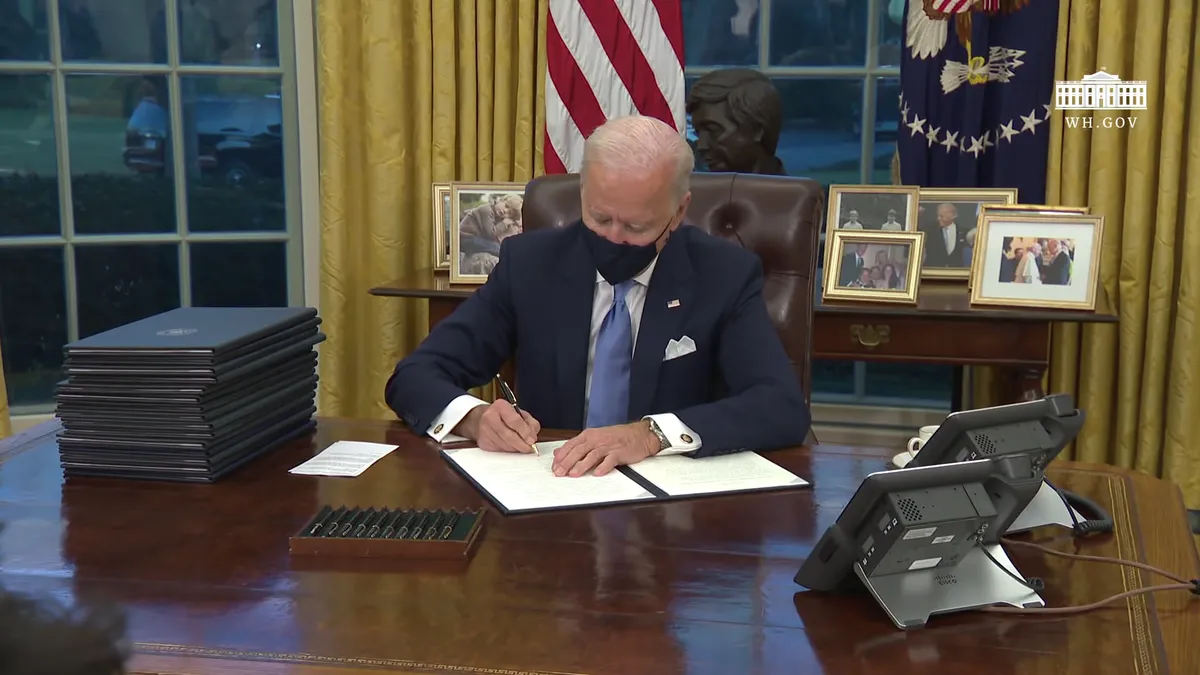
The Biden administration has put more testing at the center of its plans for controlling and exiting the COVID-19 crisis. However, tensions that predate Biden's inauguration present obstacles.
Health insurers and labs have rowed over who is to blame for gaps in coverage and rises in the price of tests, and states have opted against taking up the option to cover uninsured testing under Medicaid.
HHS data shows $1.9 billion has been paid out of the $2 billion to cover uninsured testing.
With the fund running dry, ACLA president Julie Khani wants the administration to "use the Provider Relief Fund or transfer such appropriations to the Uninsured Test Fund, as needed, and as authorized through the administrative discretion granted by Congress."
The fund has supported testing in states that opted against expanding Medicaid eligibility to the uninsured for COVID-19 diagnostics. That option, which is fully funded by the federal government, is provided by The Families First Coronavirus Response Act. However, many states have relied on the $2 billion fund instead amid reports that the Medicaid-based approach is cumbersome.
Khani voiced support for "Biden's directive to federal agencies to clarify insurers’ obligation to cover COVID-19 testing" but warned that ACLA members are still seeing claims denied.
The letter is light on specifics about the actions ACLA wants to see. Others such as the the USC-Brookings Schaeffer Initiative for Health Policy have given more detailed assessments of the loopholes and how to close them. Writing in Health Affairs earlier this month, academics set out their plan to close out-of-network loopholes.
"Congress should mandate that private insurers pay out-of-network labs and facilities three or four times average in-network prices for COVID-19 tests. In turn, out-of-network providers should be prohibited from balance billing patients," Loren Adler and Sabrina Corlette wrote.
They contend that the Biden administration's push for broader coverage of testing makes fixing out-of-network loopholes all the more imperative.
AHIP, which represents payers like Aetna, Anthem and Humana, released data in November it said showed price gouging by out-of-network COVID-19 test providers. Their survey of health insurers found almost half of out-of-network claims for PCR tests cost $185 or more, well above the average of $130 charged by in-network providers. AHIP has called on Congress to set a "reasonable market-based pricing benchmark" for out-of-network tests.