Dive Brief:
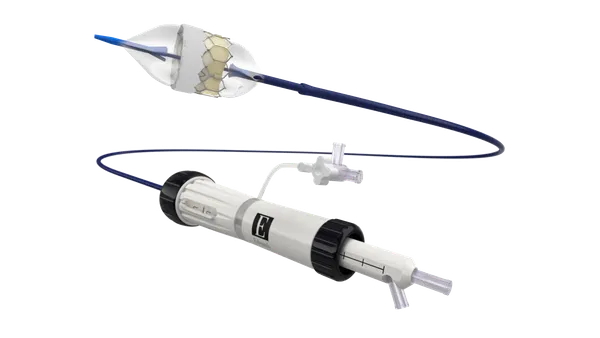
- Catheter ablation is better than antiarrhythmic drugs at cutting heart failure risk as a second-line treatment for atrial fibrillation patients, according to a retrospective study funded by Johnson & Johnson.
- The study, which was published in Heart Rhythm O2, compared the incidence of heart failure in a claims database to evaluate whether patients who have previously tried an antiarrhythmic drug should receive catheter ablation or a different medicine.
- Across a dataset of more than 18,000 patients, people who received catheter ablation had a 57% lower risk of developing heart failure than their counterparts on antiarrhythmic drugs.
Dive Insight:
In 2019, a randomized clinical trial funded by the National Institutes of Health and medtech companies including J&J’s Biosense Webster found catheter ablation is no better at reducing the composite risk of death and major cardiovascular events than antiarrhythmic drugs. However, the trial linked ablation to a lower risk of death or cardiovascular hospitalization, and other studies have found the intervention has benefits.
The lack of trials comparing the effect of catheter ablation and antiarrhythmic medicines on the risk of new-onset heart failure in atrial fibrillation patients led J&J to fund a retrospective study. The researchers used the Optum Clinformatics database to compare the effects of the two interventions.
In matched cohorts of more than 9,000 patients, the researchers linked catheter ablation to a statistically significant 57% reduction in the risk of heart failure compared to antiarrhythmic drugs. The reduction in risk was consistent across race/ethnicity and sex categories evaluated in the study.
“For the many millions of patients impacted by AFib and the clinicians who treat them, these results provide compelling decision-making evidence for effective AFib treatment options when considering the incidence of new onset heart failure,” Saima Karim, assistant professor at Case Western Reserve University School of Medicine and primary research partner in the study, said in a statement.
The study has limitations, though, as Karim and the other authors discuss in the paper. The study was a retrospective analysis and only included patients who had previously tried antiarrhythmic drugs. It is unclear if catheter ablation reduces risk in first-line patients. Another limitation was the exclusion of patients who had undergone certain cardiovascular procedures in the previous 12 months.