The Environmental Protection Agency finalized new regulations in March that will enforce tighter regulations on ethylene oxide, one of the most common sterilants for medical devices. The final rule is designed to reduce emissions of EtO, a carcinogenic gas, from commercial sterilizers by more than 90%.
Anticipating the new rule, industrial sterilizers have been upgrading emissions controls and looking at other chemicals. Medtech trade group Advamed has warned that new regulations on EtO emissions could limit capacity for sterilizing medical devices, potentially creating shortages. However, proponents of other technologies have said they can meet some of the industry's sterilization needs.
“The reality in our mind is that there are a number of products today that could be sterilized with another modality,” said Tony Eisenhut, CEO of Novasterilis, which makes sterilization equipment using supercritical carbon dioxide.
Experts said no individual technology can currently replace EtO, but a patchwork of alternatives could help reduce emissions.
The current state of device sterilization
Once manufactured, medical equipment goes through a process to ensure that it’s safe to use and doesn't pose an infection risk to patients. The Food and Drug Administration’s Center for Devices and Radiological Health evaluates sterilization methods before devices go to market.
The most common method is EtO, used for about half of all devices, followed by gamma radiation, which is used for about 40% to 45% of devices, said Aftin Ross, deputy director for the Office of Readiness and Response in CDRH’s Office of Strategic Partnerships and Technology Innovation. Both methods can process large quantities of product, but they also come with significant challenges.
EtO, a flammable gas used to sterilize materials that aren’t compatible with radiation, heat or steam, is carcinogenic to humans when inhaled. Because of this, facilities must maintain emissions equipment, and products must go through an off-gassing process to ensure no residual EtO remains.
“That is really one of the challenges we have right now. There's not currently a method that has the same scope and scale of EtO.”

Aftin Ross
Deputy Director for the Office of Readiness and Response in CDRH’s Office of Strategic Partnerships and Technology Innovation
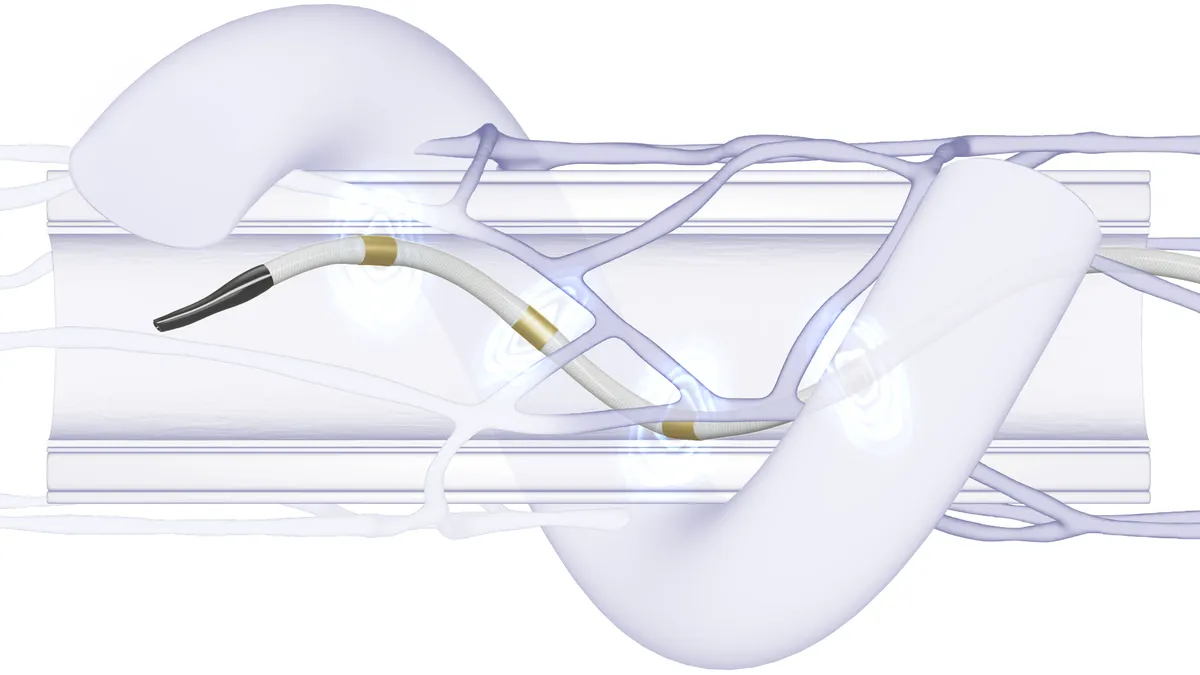
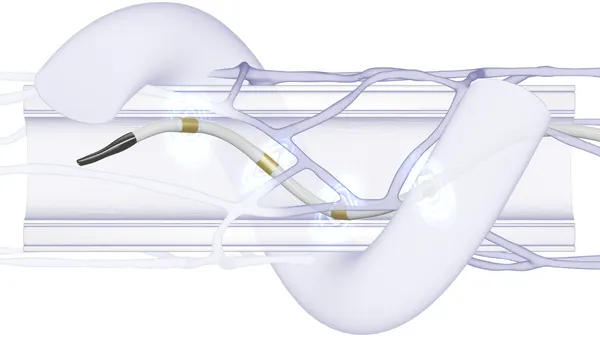
EtO is often used for polymer resin-based products, single-use medical devices, procedure kits, surgical trays, synthetic gowns, and sealed combination drug-devices like syringes and stents, according to a regulatory impact analysis for the EPA’s final rule.
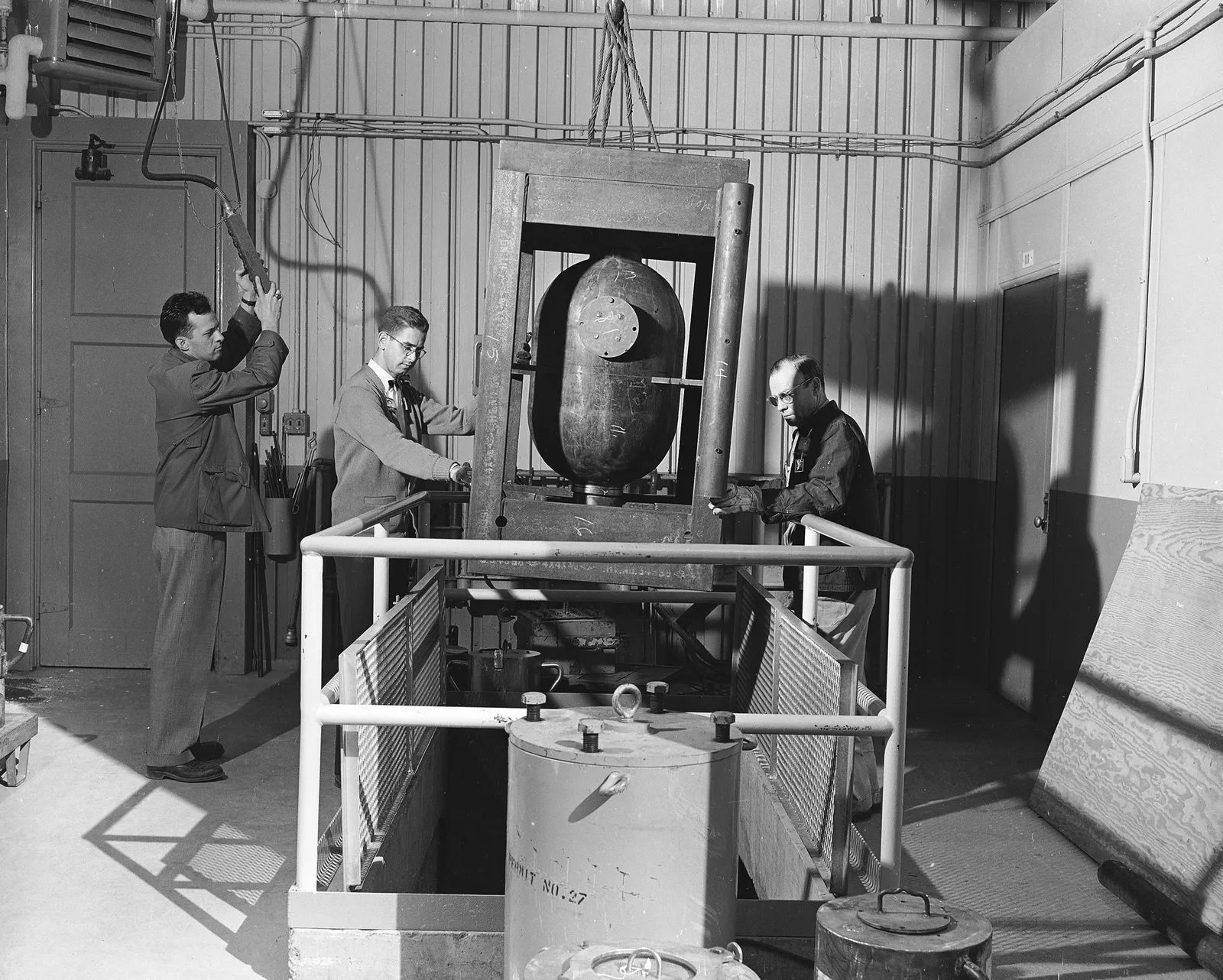
Gamma radiation relies on a byproduct from nuclear reactors, called cobalt-60. Cobalt absorbs radiation from a nuclear plant, and is then encapsulated in stainless steel "pencils," before it is transported in reinforced containers.
At a sterilization plant, the radioactive material is contained in a bunker, and the resulting radiation is used to sterilize medical devices, including gloves, gowns, syringes and surgical staplers. This process requires careful planning, as the global supply of cobalt-60 is limited, and facilities must meet strict security requirements due to the presence of the radioactive material.
“In the ‘50s, when this really came about … nuclear was on the rise,” said Andrew Patton, CEO of Nextbeam, a company that uses electronic beam radiation for sterilization. “The number of nuclear plants that produce radioactive cobalt-60, which is really the key source ingredient to running a gamma plant, hasn't evolved in the same way that we thought it might have in the ‘50s or ‘60s.”
Nordion, a subsidiary of Sotera Health, provides cobalt-60 and gamma radiation systems for medical devices and cancer treatment. Sotera CEO Michael Petras told investors in February that the company is working with Ontario Power Generation to develop a supply of cobalt-60 to support long-term growth. Roughly half of the world’s cobalt-60 is produced in Ontario, Canada, according to Nordion.
FDA searching for alternatives
The FDA started tracking facility closures in 2019, when multiple facilities using EtO shut down in response to lawsuits or state orders. That year, the agency also launched two innovation challenges to identify new sterilization methods and reduce EtO emissions.
“Our number one learning is that there is no one-size-fits-all solution,” Ross said. “We're going to continue to take a multi-pronged approach to try to reduce EtO emissions.”
Some of the alternatives explored by the challenge participants include vaporized hydrogen peroxide, nitrogen dioxide and supercritical carbon dioxide. Ross said the agency is seeing device manufacturers start to work collaboratively with sterilizers to validate new or different sterilization methods and how feasible it would be to scale up those methods.
“That is really one of the challenges we have right now,” she said. “There's not currently a method that has the same scope and scale of EtO.”
Some factors manufacturers might consider when adopting a new sterilization method include whether it is compatible with their device’s design. For example, EtO is frequently used because it’s compatible with a wide range of materials and designs with complex geometry. It’s also used for surgical kits, which often contain devices made of multiple materials.
Packaging is also an important step. In the case of EtO, devices must be sealed in gas-permeable packaging. Vaporized hydrogen peroxide is not compatible with materials made out of cellulose, such as cardboard, meaning companies might not be able to sterilize devices in the final packaging, Ross said.
The manufacturing process must also be considered. For EtO, devices are normally shipped to a separate facility to be sterilized, while some other methods allow sterilization to be done in line with manufacturing.
Ross said the FDA is considering several approaches “because even if you are only able to move a small volume of products to a particular modality — maybe one product can go here, one product can go there — cumulatively, they can have a greater impact.”

Vaporized hydrogen peroxide
One alternative being considered by medical device companies is vaporized hydrogen peroxide. It has been used for a long time in hospitals to clean reusable devices. The FDA recently recognized vaporized hydrogen peroxide as a Category A sterilization method, making it easier for device companies to use it as a sterilant in manufacturing settings.
Steris and a Stryker subsidiary are two innovation challenge participants looking at the technology.
It works by diffusing hydrogen peroxide vapor in a vacuum chamber. Afterwards, the vapor breaks down into oxygen and water, so it’s not harmful, said Maryam Tabrizian, a professor of biomedical engineering at McGill University.
This sterilization method works well for temperature-sensitive devices, pre-filled syringes, implants and devices with electronics, according to Steris. However, the method is incompatible with cellulose-based and other highly absorbent materials, which is a big challenge.
Nitrogen dioxide
Another gas-based sterilant in the challenge was nitrogen dioxide, a specialty of the company Noxilizer. Nitrogen dioxide gas is pumped into a sterilization chamber with humidity and air, and then pressurized. Chemical reactions form nitric oxide, which kills microorganisms by degrading their DNA, said David Opie, Noxilizer’s senior vice president of research and development.
One of the first niches where nitrogen dioxide has found commercial use has been with drug-device combination products, such as pre-filled syringes and auto-injectors, Opie said.
“It is a unicorn to think we're going to find a drop-in replacement for ethylene oxide sterilization. It's probably going to be a mix of a couple of alternative technologies.”

David Opie
Senior Vice President of Research and Development for Noxilizer
Noxilizer’s sterilization process runs at a lower temperature, which makes it a good fit for those products. It also can operate at a higher minimum pressure than some alternatives, meaning that when gas is removed from the vacuum chamber, it’s less likely to move the piston component of the syringe. Opie also sees custom, 3-D printed orthopedic devices as a good use case because less time is needed to aerate the product than with EtO.
Despite these advantages, Opie still doesn’t see nitrogen dioxide replacing EtO.
“It’s my opinion that medical device manufacturers will probably be using alternative sterilization — chlorine dioxide and hydrogen peroxide and [nitrogen dioxide] — for new products,” he said. “It just doesn’t seem like there is the economy to take a product currently sterilized with ethylene oxide and move it over.”
The biggest concern with switching to a new method is capacity. Currently, Noxilizer has five sterilization chambers that can process one pallet at a time, although the company can make two- to three- pallet chambers or larger.
“We’re making more now, but it will take years for that capacity to grow,” Opie said. “That’s one of the challenges for alternative sterilization, is the rate that capacity can come online to make an impact.”
Supercritical carbon dioxide
Novasterilis, a firm that offers supercritical carbon dioxide technology for sterilization, also participated in the FDA’s innovation challenge. The company was founded in 2000 based on technology from the Massachusetts Institute of Technology, CEO Eisenhut said.
The technology works by pressurizing carbon dioxide until it turns into a supercritical fluid, which can get through porous material. A peracetic acid-based solution is also added in as a sterilant.
At the end of a sterilization cycle, the residuals are minimal to undetectable, and the product is usable, Eisenhut said.

Products made with multiple materials, such as pre-packaged surgical kits, are one of the company’s “calling cards,” he said. However, because Novasterilis’ systems are pressure-based, they can’t process as many devices at once as EtO.
“When you get into high volumes where you’re doing hundreds of thousands of articles a day, that’s not a good application for our modality,” Eisenhut said.
Novasterilis sells its systems to manufacturers for them to sterilize products in-house. Eisenhut said going through the FDA’s innovation challenge was “transformational” in helping the company work more with regulated medical products. The first medical device using Novasterilis’ process was a hernia repair product in 2014, and there have been five clearances using supercritical carbon dioxide sterilization since 2020.
Eisenhut doesn't expect EtO to go away completely, but he said alternatives would be needed as medical devices become more intricate.
“The adoption cycle is slow,” he said. “A lot of it has to do with the fact that industry likes to mitigate risk and doing anything different is adding some level of risk.”
Other types of radiation
Medical device companies are also looking at other types of radiation for sterilization, such as electron beams and X-rays.
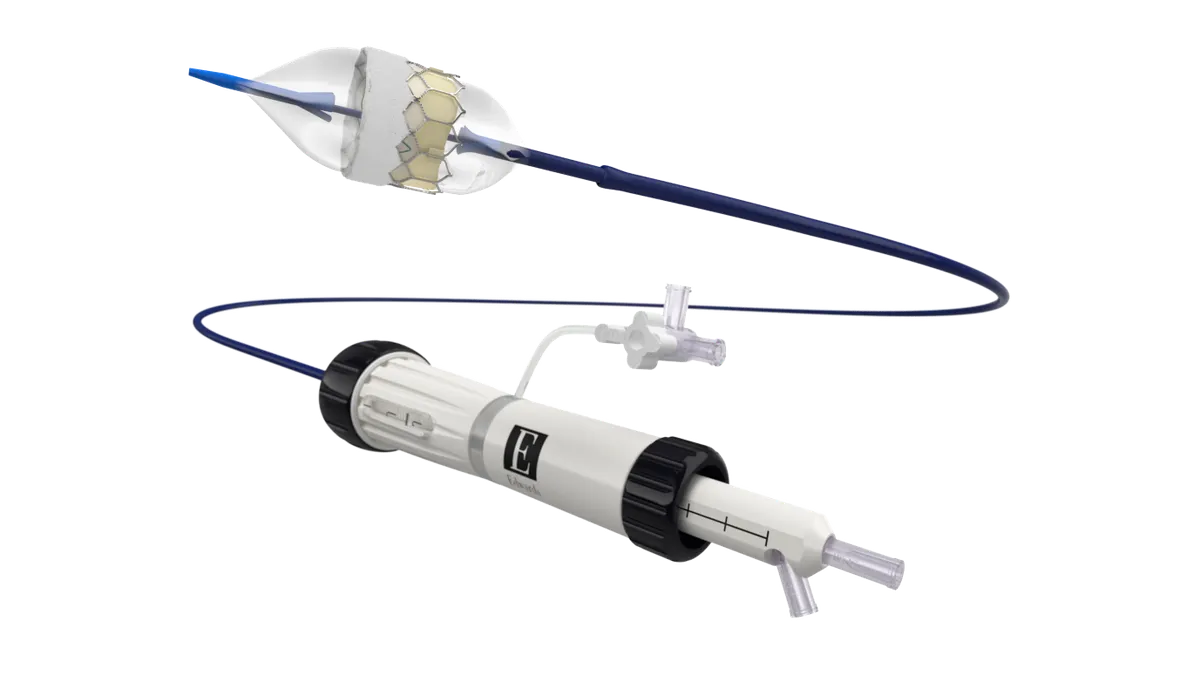
E-beam radiation has been around since the ‘50s and makes up just 5% of the total sterilization market, said Nextbeam’s Patton. He founded the startup in 2020 and built a $20 million sterilization facility in North Sioux City, South Dakota.
The technology uses a linear particle accelerator, and medical devices are moved through a “curtain of high-speed electrons,” which produces radiation throughout the product, Patton said.
E-beam technology has become more reliable and has been able to process more devices in the past decade, he added.
“For a long time, [EtO] and gamma were really cheap, and it was really hard to compete,” he said. “When you had cheap [EtO], and there was no perceived environmental risk, and you had cheap gamma, and there was no perceived supply shortage, there was no real reason to compete with it.”
People have started investing more in e-beam as other sterilization methods have increased in price and decreased in availability, Patton said.
Some products currently sterilized using EtO could be moved to e-beam, but there are a few challenges. For example, radiation degrades teflon, which is used in devices where things need to slide together smoothly.
Packaging is also a concern — because e-beam uses large particles, it doesn’t have the same depth of penetration as other modalities. Patton used the analogy of cooking a steak: if it’s too thick, the center part might not get warm enough.
While X-ray could be used to sterilize a whole pallet of devices at a time, e-beam can go about one or two boxes deep, he said.
More commercial sterilizers are also looking into X-ray technology. Steris outlined plans to add two U.S. sites this year in Chicago and Ontario, California, CEO Dan Carestio told investors in February.
Patton said there’s a lot of interest in X-ray sterilization, but it’s less efficient, requiring more power and a larger facility than e-beam radiation. The technology is also less mature. Still, Patton said he would like to open an X-ray facility one day.
The future of sterilization
Some companies are using programs offered by the FDA to switch to other sterilization methods.
CDRH’s Ross said the FDA has seen several innovation challenge participants also start to participate in master file pilot programs the agency is offering that make it easier to switch to another sterilization method. Currently, three master file programs around sterilization are open to participants.
Steris’ Carestio told investors in November that the company was participating in a master file pilot program that would allow its customers to switch between different modes of sterilization, “whether that's [EtO] to X-ray, or gamma to X-ray, or even e-beam to gamma,” without having to file for a new 510(k).
“It lowers a significant regulatory hurdle, I would say, that allows customers to build in much more resiliency and also switch between technologies,” he said.
Looking forward, proponents of EtO alternatives see a future, even if it’s slow going.
“It is a unicorn to think we're going to find a drop-in replacement for ethylene oxide sterilization,” Noxilizer’s Opie said. “It's probably going to be a mix of a couple of alternative technologies.”