Dive Brief:
-
The head of FDA's device unit outlined why the agency is putting additional funding toward postmarket surveillance initiatives in an article published this week, co-authored by the executive director of the National Evaluation System for health Technology (NEST). FDA's 2019 budget included $51 million earmarked for the program.
-
The NEST Coordinating Center, led by Rachael Fleurence, is aiming to collect real-world evidence to inform decisions about medical devices across their life cycles, including in the assessment of the safety of products on the market.
-
CDRH chief Jeff Shuren said FDA thinks the active surveillance approach to postmarket safety enabled by NEST's work can improve on its existing systems if its data quality framework being developed can achieve FDA evidentiary standards. Ultimately, Shuren and Fleurence suggest the system has the potential to "impact regulatory, clinical, and coverage decision making in the United States and improve the health and the quality of life of patients."
Dive Insight:
FDA wants to cut the time it takes to bring medical devices to market without compromising patient safety. A timely, efficient postmarket surveillance system could support that goal by giving FDA a full, up-to-date picture of the safety of devices in real-world use.
However, the limitations of existing surveillance systems are hindering efforts to improve postmarket oversight. Postapproval studies of devices are difficult to enroll, and the current passive surveillance system suffers from the under-reporting of adverse events. To compound matters, many reports FDA does receive are incomplete.
FDA helped get NEST started in 2016 to address these and other issues. Recently, the agency put up more money specifically to further NEST's work on the active surveillance of medical devices.
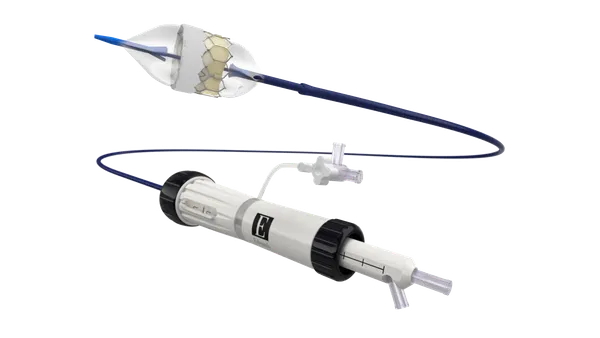
Writing in the journal Clinical Pharmacology and Therapeutics, Shuren and Fleurence detailed the aforementioned limitations of passive surveillance before outlining how NEST plans to better these systems. The paper cited a FDA-funded study that used active surveillance of a clinical registry to quickly identify safety signals in patients treated with an implantable vascular-closure device.
That study convinced FDA of the potential of active surveillance but left unanswered questions about how to apply the model to routine regulatory oversight. The NEST funding is intended to clarify the path to widespread use, for example by showing how the approach can be scaled to cover a large number of devices.
In November 2018, the agency announced eight test cases to evaluate NEST's ability to utilize real-world evidence. Abbott and Johnson & Johnson are among companies taking part in the test cases, most of which are observational. For example, three test cases relate to monitoring the safety of orthopaedic devices using electronic health records.
"Although the current set of NEST test cases use observational designs, randomized studies at the point of care that leverages electronic health data to identify, and follow‐up patients are possible and an objective of NEST," Shuren and Fleurence wrote. "Through additional funding from the FDA, active surveillance of medical devices leveraging RWD in health systems will be a key area of focus for NEST in 2019."
Through its activities, NEST aims to address some of the barriers to the effective use of real-world data. Challenges listed by Shuren and Fleurence include how to aggregate and analyze data from multiple sources. NEST has established expert committees to find answers to such questions.
NEST's founding network collaborators include Mayo Clinic, Anthem, Duke University Health System, Mercy Health and others. The agency has suggested that eventually, NESTcc will move towards a model where companies pay to use the system to conduct real-world evidence studies to maintain the financial viability of the system.