Dive Brief:
- HHS Secretary Xavier Becerra on Wednesday sent a letter to healthcare providers and insurers reminding them that COVID-19 vaccines and testing must be free without charge for patients.
- The agency said Becerra issued the warning following recent reports of Americans facing costs associated with coronavirus vaccinations and tests. Becerra's letter forcefully states that group health plans and health insurers are legally required to cover coronavirus diagnostic tests without cost-sharing, and that those who fail to comply may be reported to state insurance departments or to CMS for possible enforcement action.
- HHS, along with with the Departments of Labor and Treasury, in February issued updated guidance addressing the requirement for group health plans and health insurers regarding COVID-19 testing. However, Becerra said in Wednesday's letter that uncertainty about coverage and costs for these tests continue to create access barriers for Americans "as they decide whether to get tested."
Dive Insight:
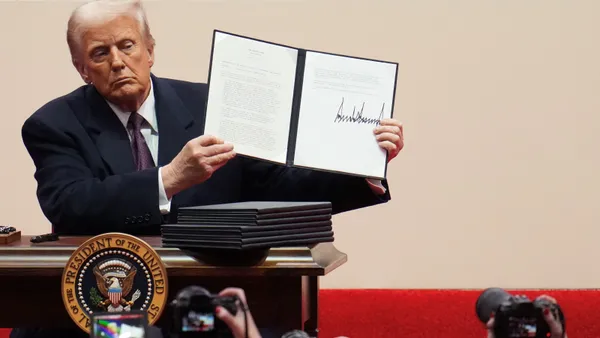
The American Clinical Laboratory Association, which has members including Quest Diagnostics and LabCorp, warned in 2020 during the waning months of the Trump administration that previous guidance from HHS-Labor-Treasury had only served to muddy what they saw as the clear coverage mandates passed by Congress that required comprehensive health plans to cover COVID-19 testing without cost sharing.
"Americans should be able to access the COVID-19 testing they need without hesitation — and without fear that a claim will be denied by their health plan," said Julie Khani, president of ACLA, in a written statement.
ACLA raised the alarm to the incoming Biden administration about patients facing a "patchwork of coverage policies that drives uncertainty and undermines federal response efforts" to the pandemic. That's when the three agencies issued updated guidance.
While the February HHS-Labor-Treasury guidance was meant to provide clarity, Becerra found it necessary on Wednesday to remind healthcare providers of their signed agreements to cover COVID-19 vaccines free of charge to patients, and group health plans and health insurers of their legal requirement to provide coverage of COVID-19 vaccinations and diagnostic testing without costs to patients.
"We will remain vigilant in holding providers accountable for vaccinating the public without charging patients and holding issuers accountable for covering COVID-19 diagnostic testing without cost-sharing," Becerra wrote.
The HHS secretary pointed out that group health plans and health insurers are also prohibited from delaying COVID-19 diagnostic testing or making it "more cumbersome and costly through prior authorization or other medical management."
Becerra warned that in addition to reporting bad actor health plans and insurers for non-compliance to CMS or state insurance departments, the Department of Labor would also address any complaints regarding coverage offered in connection with private, employer-sponsored group health plans.
HHS last month announced it was dedicating $4.8 billion from the American Rescue Plan to continue reimbursing healthcare providers for testing uninsured individuals for COVID-19 through a Health Resources and Services Administration program. ACLA had urged the Biden administration to replenish the uninsured fund.
"Continued access to, and coverage of, high-quality COVID-19 testing remains critically important for all Americans, regardless of insurance status," ACLA's Khani said in a statement. ACLA's member labs have performed more than 125 million coronavirus PCR tests to date.