Dive Brief:
-
Researchers at genetic testing company Illumina and leading cancer hospitals have used a liquid biopsy to detect cancer-driving mutations in patients who lacked analyzable tissue samples.
-
The noninvasive next-generation sequencing assay identified mutations in around 25% of the patients without analyzable tissue samples, suggesting it can play a role in informing treatment decisions in some circumstances.
-
However, the inability of the test to detect some mutations in patients with analyzable tissue samples is likely to limit near-term applications of the approach.
Dive Insight:
The potential to detect and characterize cancer from fragments of circulating tumor DNA has turned the liquid biopsy space into one of the most hyped corners of the medtech industry. Guardant Health raised $238 million through an IPO last year and has since presented data suggesting its blood test is as good at detecting therapeutically-targetable genomic alterations as standard tissue biopsies.
Elsewhere, Illumina-spinout Grail has raised more than $1 billion to develop a blood test capable of detecting cancer earlier. Guardant has an early detection research program, too, but the near-term liquid biopsy opportunities revolve around selecting treatments and monitoring their effectiveness.
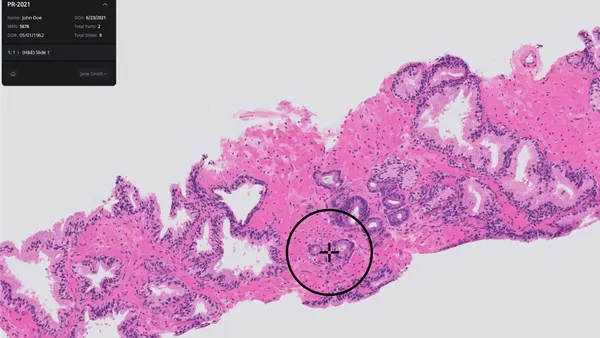
Those opportunities attracted the attention at physicians at Memorial Sloan Kettering Cancer Center (MSKCC) and other oncology institutes, who applied Illumina’s sequencing capabilities and a Grail algorithm to the analysis of blood samples taken from 127 non-small cell lung cancer patients.
The researchers lacked analyzable tissue samples for 17 of the patients and as such were unsure if a genetically-targeted cancer therapy would be effective. The liquid biopsy found four of the patients had KRAS mutations, one of which was subsequently confirmed by a tissue analysis. None of the other three patients underwent tissue biopsies. The prognostic impact of KRAS remains uncertain but the finding hints at the possibility for liquid biopsies to uncover insights that inform treatment.
Other aspects of the data are mixed, though. Two patients underwent tissue biopsies after the blood test had failed to detect a mutation. The tissue biopsies confirmed mutations missed by the blood test in both patients.
The application of the test to patients who had known cancer mutations at the time of the liquid biopsy emphasizes the problem. The test detected cancer-driving mutations in 68 of the 91 patients in that cohort, meaning it failed to identify 25% of the markers. Bob Li, a MSKCC oncology who co-wrote the paper, called the detection rate "modest."
Given the importance of detecting mutations to patient outcomes, the true positive rate could limit use of the liquid biopsy. Even so, Li thinks there may be a place for the test in diagnostic pathways.
"Our results suggest that liquid biopsy can play a complementary role to tissue biopsy in the treatment of lung cancers. Due to its high specificity of 100%, meaning there were no false positives, liquid biopsy could be performed first and be used to guide treatment, especially when tissue biopsy may be inadequate or not feasible," Li said in a statement.
As tissue biopsies take around twice as long as liquid biopsies, the blood test could provide useful early insights into the treatment of patients who may deteriorate quickly.