Dive Brief:
- A meta-analysis of 230 studies found advantages to using Intuitive Surgical da Vinci robots in cancer procedures.
- The paper published in the medical journal Annals of Surgery looked at 30-day outcomes in patients who underwent robotic, laparoscopic and open surgeries. Intuitive and Massachusetts General Hospital scientists conducted the analysis.
- Rates of postoperative complications, readmissions and death were lower after robotic surgeries than laparoscopic and open procedures. The study did not look at longer-term outcomes such as cancer-free survival.
Dive Insight:
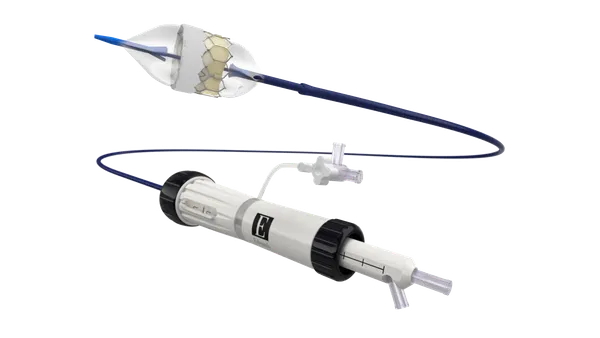
Intuitive has designed da Vinci to help surgeons navigate deep or narrow areas of the body such as the chest, abdomen and pelvis. The features are potentially beneficial to cancer surgeons. Multiple studies have compared Intuitive’s da Vinci robot to laparoscopic and open cancer surgeries but only looked at outcomes in individual tumor types.
Pooling the results of multiple studies allowed the researchers to assess outcomes across tumor types. Intuitive said in a Dec. 5 statement that the findings could be helpful for people who are considering using robotics in settings that cover multiple cancer specialties.
The meta-analysis included data from 230 studies performed in 22 countries over 12 years. The studies compared the three surgical techniques across seven procedures and four specialties. There were more than 1 million cases each of robotic, laparoscopic and open surgeries in the analysis.
Robotic cases took 17.7 minutes longer than laparoscopy and 40.9 minutes longer than open procedures, but hospital stays were between half a day and two days shorter. Blood loss was less in robotic surgeries than open procedures.
Robotic cases were less likely than laparoscopy to convert to open surgeries. Robotic procedures were also associated with a lower rate of reoperation than open surgeries, but were about equivalent with laparoscopy.
The analysis provides evidence that there are short-term benefits to using da Vinci to remove tumors. However, important outcomes that could inform the choice of procedure, such as cancer-free survival rates, are outside of the scope of the study.