UPDATE: Sept. 3, 2019: Inspire Medical Systems said it's received two additional draft local coverage determinations from Medicare contractors Novitas Solutions and First Coast Service Options that cover 12 states and the District of Columbia, allowing use of Inspire’s hypoglossal nerve stimulation device in the treatment of some cases of obstructive sleep apnea. Concurrently, First Coast canceled its existing negative coverage policy on the Inspire therapy. The proposed policies are currently in the public comment period, which is expected to be 60 days. The final LCDs are expected to be published in early 2020.
Dive Brief:
-
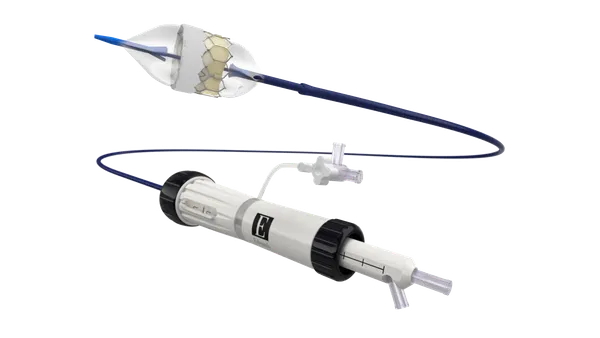
Inspire Medical received draft local coverage determinations from two Medicare contractors that cover 19 states on Aug. 22, permitting use of Inspire’s hypoglossal nerve stimulation device in the treatment of some cases of obstructive sleep apnea, potentially removing a barrier to the use of the product.
-
News of the potential Medicare coverage comes shortly after Inspire revealed private payers representing almost 18 million people agreed to reimburse its device. The new payer decisions add to existing policies covering more than 100 million people.
-
In both cases, the contractors are proposing to cover Inspire’s device in patients aged 22 years or older who have tried continuous positive airway pressure or CPAP without success and meet certain criteria, such as being below a body mass index threshold. Both policies also prohibit the use of the device in patients with conditions including severe restrictive or obstructive pulmonary disease.
Dive Insight:
Medicare contractors Noridian Healthcare Solutions and Palmetto published the draft LCDs. There are differences between the two policies but many of the key points are the same.
The comment periods on the Noridian and Palmetto draft LCDs close in October and November, respectively. If finalized without undergoing major changes, the LCDs could reduce one of the challenges Inspire has faced when trying to grow sales of its devices.
Talking to investors earlier this month, Inspire CEO Tim Herbert said physicians and centers that have wanted to use the device in patients not covered by payer policies needed to "conduct prior authorizations and appeals and peer-to-peer phone calls with medical directors." Herbert said this "limits the energy around bringing new patients into the process." The CEO also noted that "a high number of patients" in this situation "fatigue from the process" and drop out.
"If we could ease some of the burden of Medicare with some of the LCDs, that will have a real positive effect on streamlining when a patient can come in, be diagnosed, work through their insurance, schedule implant and have their implant procedure completed," Herbert said.
With the LCDs coming after positive decisions by Aetna, UnitedHealthcare and multiple other payers, Inspire said it is removing some of the constraints on the capacity of healthcare centers to use its device. Currently, top-performing centers use the device on around 50 patients a year but Herbert thinks that ceiling can double if Inspire frees them from "fatigue factors" such as prior authorization.
Inspire is already on an upward trajectory. Sales increased by 65% in the second quarter, enabling it to raise its 2019 outlook for the second quarter in a row. Inspire now expects to generate sales of up to $75 million, compared to $70 million going into 2019.