Dive Brief:
-
Merck & Co. has teamed up with Roche to develop a companion diagnostic capable of identifying patients with solid tumors positive for mismatch repair deficiency, which Merck's anti-PD-1 checkpoint inhibitor is approved to treat.
-
Keytruda's OK for treating solid tumors with mismatch repair deficiency, which describes mutations in certain genes involved in correcting mistakes made when DNA is copied in a cell, was the first tissue-agnostic cancer drug approval in the U.S.
-
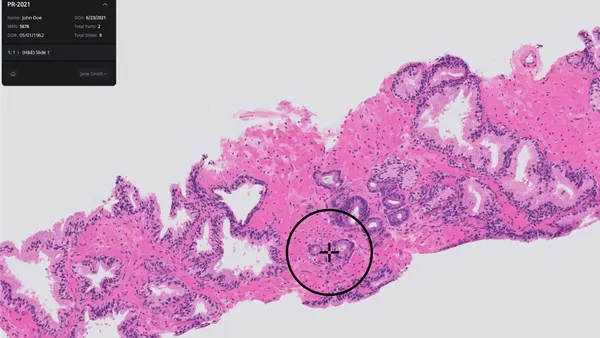
Roche will provide physicians with a way to identify these patients using an immunohistochemistry (IHC) assay — a lab test that uses antibodies to test for certain markers — that will run on its BenchMark ULTRA instrument.
Dive Insight:
Throughout the history of cancer care, the location of the tumor has driven decisions about how to treat the disease. Lung cancer was treated differently than colorectal cancer because the tumors are found in different parts of the body. However, research has shown that cancers in the same tissues can have different characteristics, and that tumors in different locations can have common features.
This research initially led to more refined, biomarker-driven approaches to treating diseases in certain organs, such as Roche's breast cancer drug Herceptin (trastuzumab). More recently, the research has led drug developers to focus biomarkers found across multiple types of tumors.
That thinking led Merck to test its checkpoint inhibitor Keytruda (pembrolizumab) as a treatment for patients whose cancers tested positive for mismatch repair deficiency, also known as microsatellite instability. Most common in colorectal cancer, mismatch repair deficiency can also be found in breast, prostate, thyroid and bladder cancers. .
Merck's clinical testing led to the FDA's first approval of a tissue agnostic drug. For a physician to prescribe a drug on the basis of mismatch repair deficiency, they need a way to assess whether a patient has this indicator of genomic instability.
Currently, physicians have access to assays that detect four MMR proteins, MLH1, MSH2, MSH6 and PMS2. Together with a test for the BRAF V600E mutation, the assays are central to the identification of patients with Lynch syndrome, a genetic condition that raises a person's risk of colorectal cancer and tumors affecting other tissues including endometrium, ovary and stomach.
After approving Keytruda for mismatch repair deficient solid tumors, the FDA identified questions about the best test and the need to identify more people with Lynch syndrome as remaining challenges. Merck's deal with Roche seeks to address these challenges by tailoring the existing assay panel to the selection of patients with solid tumors suitable for treatment with immunotherapy.
A companion diagnostic designed to serve this purpose is already in development. The IHC test will run on Roche's widely-used in situ hybridization staining platform, the BenchMark ULTRA instrument.
Roche will seek FDA approval for the biomarker panel but has yet to share a timeline for the regulatory process.