Michelle Tarver, the new leader of the Food and Drug Administration’s medical device center, faces significant challenges ahead.
Tarver is taking over as director of the Center for Devices and Radiological Health as the regulator grapples with questions around artificial intelligence in medical devices, racial bias in pulse oximeters, concerns about the recall process after Philips pulled millions of respiratory machines, and scrutiny of its former leader’s potential conflicts of interest.
Patient advocates, who have called for stronger device standards and faster, more transparent recalls, see an opportunity for change with a new director. Meanwhile, medtech companies hope to build on predecessor Jeff Shuren’s legacy of making the U.S. the go-to market for new medical devices.
“She is in a position to show a commitment to public health and safety, and possibly build that trust and confidence in the public for medical devices,” said Maria Gmitro, founder and president of the Breast Implant Safety Alliance, a nonprofit advocacy group.
Tarver’s leadership
Tarver was named permanent director last week after spending more than 15 years with CDRH. Some of her accomplishments include helping build the first patient engagement advisory committee at the FDA, developing patient-reported outcome measures, and conducting trials and surveys to capture patient preferences.
Both patient groups and device companies commended Tarver’s experience and focus on patients, describing her as thoughtful and approachable.
“She let it be known that she cared very much about patients understanding the risks and benefits of medical products, and including patients and consumer advocates in the process,” said Diana Zuckerman, president of the National Center for Health Research, a nonprofit think tank.
Madris Kinard, CEO of Device Events, a company that makes software to track adverse event reports and recalls, said Tarver has been receptive to suggestions in public meetings. For example, Tarver recently helped make certain demographic data available in the FDA’s adverse events database, which can be helpful in learning about off-label use in pediatrics.
Andrew Fish, CEO of the Medical Device Innovation Consortium, a public-private group founded in 2012, said Tarver is a respected leader in the agency and has been involved in efforts around patient input, patient engagement and clinical trial diversity.
“[Tarver is] thoughtful and direct in her engagement. She doesn’t hedge,” said Scott Whitaker, CEO of medtech lobbying group Advamed, adding that Tarver’s time as a regulator and a physician brought a personal gravitas to her proposals.
Transition from Shuren
Tarver seemed poised to lead the device branch in July, when she was named acting director when Shuren stepped down after leading CDRH for 15 years. Shuren plans to leave the agency later this year.
House Democrats have called for an investigation into Shuren’s tenure after a New York Times report found Shuren’s wife, Allison Shuren, worked as legal counsel for medtech companies while he led CDRH. The FDA told MedTech Dive in August it found no evidence that Shuren violated the criminal conflict of interest statute or that regulatory decisions were affected by Allison Shuren’s employment.
One of the concerns raised in the report was that Allison Shuren’s firm worked on an acquisition of Allergan as the FDA asked the pharmaceutical company to recall certain models of breast implants for the risk of developing a type of lymphoma.
“It’s concerning reading about the timeline of the Allergan breast implant recall and Dr. Shuren’s wife being a part of the law group that was involved in the sale of Allergan to Abbvie,” Gmitro said. “It doesn't build a lot of trust.”
The Department of Health and Human Services’ Office of Inspector General said it does not have an update to share publicly on whether an inquiry will be opened into Shuren’s tenure.
Michael Abrams, senior health researcher at Public Citizen, said an investigation is warranted to “advise and alert” Tarver to existing and future conflicts.
Advamed’s Whitaker and MDIC’s Fish both spoke highly of Shuren’s legacy. Fish said the former CDRH director was passionate about bringing innovations to patients “as fast as possible, without compromising safety and effectiveness.”
Whitaker cited CDRH’s collaboration with the industry under Shuren. Whitaker also praised the budget, workforce and process improvements during the user fee process, where the FDA sets how much money it can receive from industry in fees based on hitting review timelines and staffing milestones.
“One of his goals was to try to position the U.S. as the primary market for medical technology globally,” Whitaker said. “And everyone would agree he succeeded.”
Future priorities
Tarver outlined some of CDRH’s priorities during a keynote at Advamed’s The Medtech Conference in mid-October. She spoke about the importance of listening to patients, based on her experience as an ophthalmologist.
“It ties directly into the vision of our center,” said Tarver, who still works with patients. “We put people in the U.S. first, and we want them to have access to high quality, safe and effective medical devices of public health importance first in the world.”
She called out three strategic priorities for the center: promoting a modern and diverse workforce, making the organization more agile and resilient to be prepared for future challenges, and advancing health equity.
Tarver will also lead CDRH through the next round of user fee discussions in 2027. The fees made up more than a third of the agency’s budget in 2022, according to HHS.
Per the 2022 agreement, CDRH would receive a minimum of $1.78 billion in fees between 2023 and 2027, with potential increases if certain performance goals were met. In exchange, the regulator agreed to make decisions on medical device submissions within a specified number of days and meet certain hiring goals.
The FDA was authorized to collect about $335.8 million in medical device user fees in fiscal 2024, before an inflation adjustment.
Advamed’s Whitaker wants to see the fundamental structure of the latest round of user fee agreements remain intact and continued progress on review timelines.
“We want to make sure we don’t change course dramatically,” Whitaker said. He also expects AI will be a part of the next round of user fee discussions.
GE Healthcare CEO Peter Arduini said in an emailed statement that ensuring the review process for these technologies is clear and consistent “will be paramount.”
Patient groups, on the other hand, see the user fee process as giving industry too much of a voice in the FDA’s activities. Abrams would like the FDA to get more funding from Congress and less from industry.
Advocates have also called for more input into the negotiations between the FDA and industry leading up to the agreement. Those discussions are not open to the public and have been criticized for a lack of transparency. The FDA is required to hold meetings with patient groups and outside experts during user fee negotiations, but the discussions are separate from talks with industry.
“None of the rest of us are allowed in. … No patient groups, no consumer groups, no academic researchers, nobody else,” Zuckerman said. “It’s all behind closed doors, and we’re all shut out of the process.”
In the most recent round of user fee discussions, the FDA held two public meetings with patient groups, an open public session with patient speakers, and 13 additional consultation meetings that included patient or consumer organizations, FDA spokesperson Kristina Wieghmink wrote in an email.
Before the next negotiation period, the FDA will notify the public about speaking opportunities, Wieghmink said.
Focus on device safety
Patient advocates also called for stronger premarket review of devices. The majority currently go through the FDA’s 510(k) pathway, a less rigorous process where devices need to demonstrate they’re substantially equivalent to predicate devices, or products already on the market. The FDA has proposed changes in draft guidance, such as recommending devices not be based on a predicate that was recalled for design reasons.
Those changes are not enough, Zuckerman said. Higher-risk devices that go through more scrutiny under the FDA’s premarket review process often still submit data from single-arm trials without a control group, Zuckerman said.
Zuckerman added that it doesn’t make sense for the highest-risk medical devices to have lower evidence standards than low-risk prescription drugs.
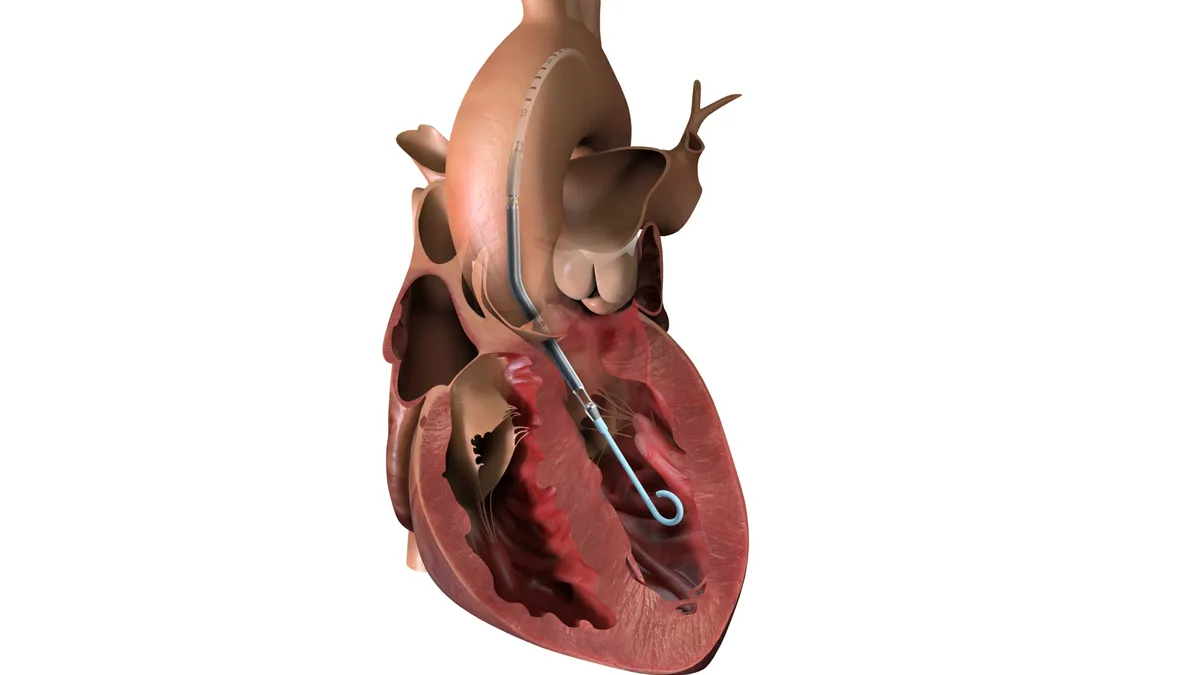
“Something for tummy aches shouldn’t be going through a more rigorous process than a cardiac implant,” Zuckerman said.
Patient groups also called for stronger oversight after devices are on the market, as well as faster, more transparent recalls. They also called for broader adoption of unique device identifiers to ensure recalls are efficient and for less reliance on voluntary recalls.
“It’s great if we’re getting innovative devices to market faster. I understand people wanting to try new devices, especially if there are no other alternatives,” said Device Events’ Kinard. “But the FDA needs to be just as quick to act and recall a device when they find a problem.”