Dive Brief:
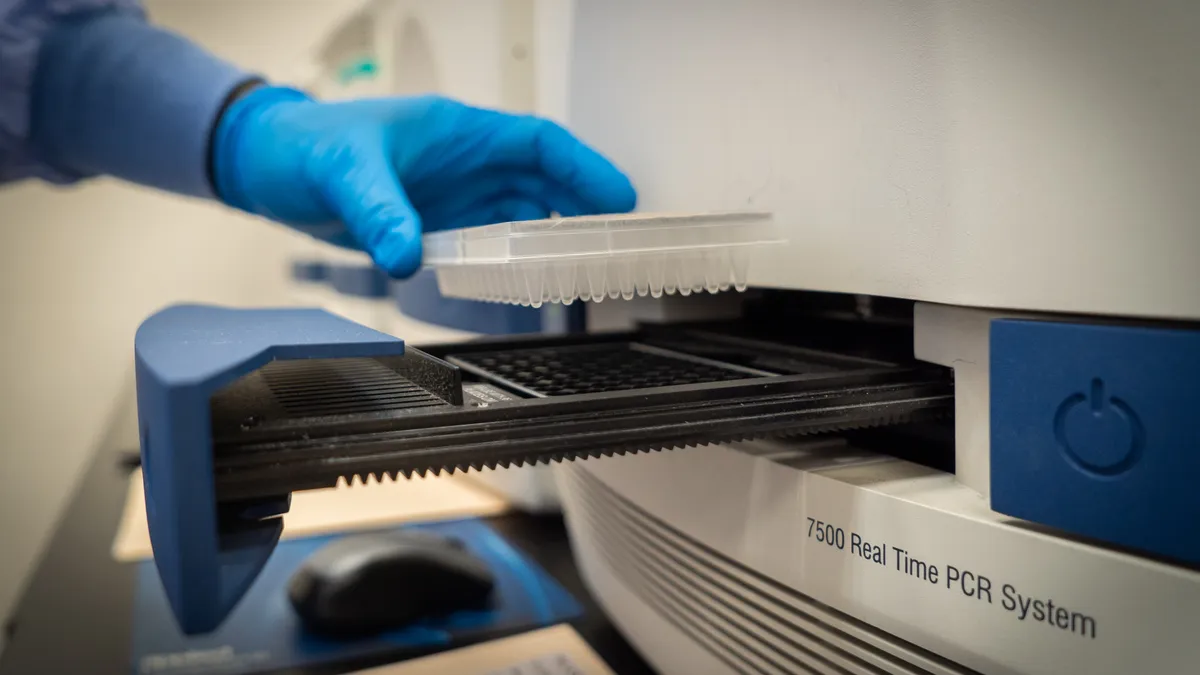
- A Quest Diagnostics coronavirus test is the first authorized by FDA for sample pooling, a method meant to screen more people using fewer resources, the agency announced Saturday.
- The product OK'd for use with the technique, Quest's SARS-CoV-2 rRT-PCR test, first got emergency use authorization by FDA on March 17. The company said it will begin leveraging the method at labs near Washington, D.C. and Boston by the end of this week, planning to expand it to other sites later.
- Although the pooling technique may help stretch testing resources, "it is not a magic bullet," Quest's chief medical officer Jay Wohlgemuth said in a statement Saturday, adding that "testing times will continue to be strained as long as soaring COVID-19 test demand outpaces capacity."
Dive Insight:
The regulatory development on sample pooling is the latest evolution in the scaling of U.S. coronavirus testing and comes amid test turnaround times at the major lab companies extending past multiple days.
Quest was among the first private companies in mid-March to have a molecular test OK'd by FDA, following Roche, Thermo Fisher, and LabCorp. Since then, FDA has looked to make more convenient testing options available, authorizing a number of test kits for at-home sample collection, the first that uses a saliva specimen, and a few diagnostics that test for both COVID-19 and the flu.
The FDA nod for the latest type of testing is meant to more efficiently use testing resources. Quest said last week its average turnaround time for coronavirus test results for non-priority patients is at least a week, thanks to surging demand in the South, Southwest and West, with no indication supply pressures would soon improve. Slow results diminish the potential impact of contact tracing, experts say.
But rival LabCorp said in an update Sunday its average wait time is now three to five days from the time of specimen pickup, down from the four to six days reported two weeks ago.
FDA describes sample pooling as using a single test to assess specimens from multiple individuals. The Quest test is authorized to assess specimens from four people at once. If a test used to assess that combined "batch" of specimens returns a positive result, then it's best practice to retest each of those people individually. If a pooled test comes back negative, then individuals don't need to be retested, and a lab will have saved resources.
Quest used data from 3,091 specimens among a population with virus prevalence between 1% and 10% to back its application. It found none would have been falsely deemed negative if pooled, a conclusion FDA backed in its statement.
However, the technique may not be effective in current COVID-19 hotspots given the high positivity rates. More than a dozen states, a Puerto Rico, have positivity rates topping 10%, according to data compiled by Johns Hopkins University. Arizona, for example, has a positivity rate nearing 24%, with Florida close to 19%, according to the tracker.
Regulators acknowledge the technique is most useful in areas where prevalence of the virus is already expected to be low, and negative results are more likely.
"Sample pooling becomes especially important as infection rates decline and we begin testing larger portions of the population," FDA Commissioner Stephen Hahn said in the agency's statement Saturday. That's not yet realistic in all parts of the U.S.
Quest is set to report second quarter financial results before market open Thursday. The company previewed those results last week, tallying a better-than-expected 6% decline in revenue. Depressed routine testing volumes improved as the quarter progressed and huge demand for COVID-19 tests helped make up some of that difference.