Dive Brief:
-
The Journal of the American Medical Association on Monday published full details of one of the studies that appeared to slow growth in sales of Abiomed’s Impella devices late last year.
-
Supported by FDA, Mayo Clinic, Yale, and others, the analysis of registry data from 2015 to 2017 links Impella use to higher rates of in-hospital major bleeding and death than intra-aortic balloon pumps.
-
While Abiomed has questioned the reliability of the results, the authors of an accompanying JAMA editorial argue the study supports “a more restrictive use” of Impella.
Dive Insight:
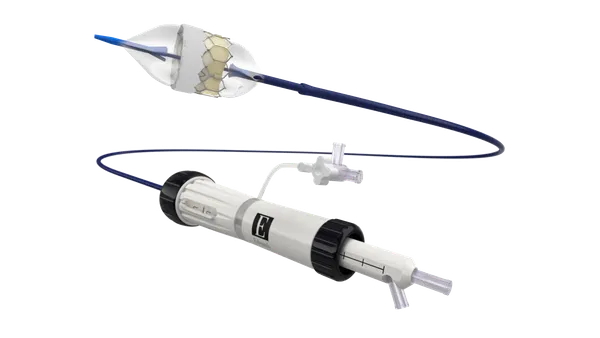
Abiomed was rocked late last year by two presentations at the American Heart Association's 2019 Scientific Sessions. The observational studies suggested Impella is associated with worse health and financial outcomes than intra-aortic balloon pumps (IABPs), sending Abiomed shares down 10% and causing a slowdown in sales growth that led revenue to fall short of expectations.
The JAMA paper published this week largely reiterates the findings presented last year, most notably the headline takeaway that Impella is associated with a higher risk of in-hospital death than IABPs. In an analysis of 1,680 propensity-matched pairs taken from two registries, the risk of in-hospital death associated with Impella was 45%, as compared to 34% in the IABP cohort. The researchers also linked Impella to 31% risk of in-hospital major bleeding, as compared to 16% in the IABP group.
Abiomed has gone on the offensive against the study and another AHA presentation that called the value of Impella into question.
Talking to investors earlier this month, Abiomed CEO Michael Minogue asserted that both publications “contain factual inaccuracies that demonstrate a lack of knowledge of the totality of the Impella data and FDA regulatory process.” An editorial released alongside the other paper, published in Circulation at the end of January, also found limitations with the study.
In an editorial published alongside the JAMA study Monday, German physicians acknowledged the potential for certain factors to explain the divergent outcomes, explaining that “findings derived from observational registries may be limited by selection bias and confounding, which cannot be completely accounted for even with sophisticated statistical matching and analyses.”
The editorial also echos earlier calls for the need for a randomized controlled trial. Still, the authors think the study should inform clinical practice.
“The study by Dhruva et al, together with other registry studies, provide evidence to support a more restrictive use of these devices and as based on current guidelines, only in selected patients with refractory cardiogenic shock,” the authors wrote.
If that cautious view is adopted by physicians, Abiomed may face a headwind until it has results from randomized controlled trials that refute the findings of the observational studies. Abiomed is working to generate those results, outlining plans recently to start a “wave of clinical trials” intended to get a strong recommendation for Impella in clinical guidelines.
Ultimately, the JAMA paper concludes that "Further research may be needed to understand optimal device choice for these patients," and investigator Joseph Ross wrote on Twitter Monday that the real-world evidence-focused National Evaluation System for health Technology Coordinating Center may play an "important role" as long as "trial data remain inconclusive."
This is the opportunity for real-world data - can these data be used to characterize device safety and effectiveness when trial data remain inconclusive, or enhance our understanding of how devices perform in clinical practice? Important role for @NESTccMedTech and others (4/9)
— Joseph Ross (@jsross119) February 10, 2020