Dive Brief:
-
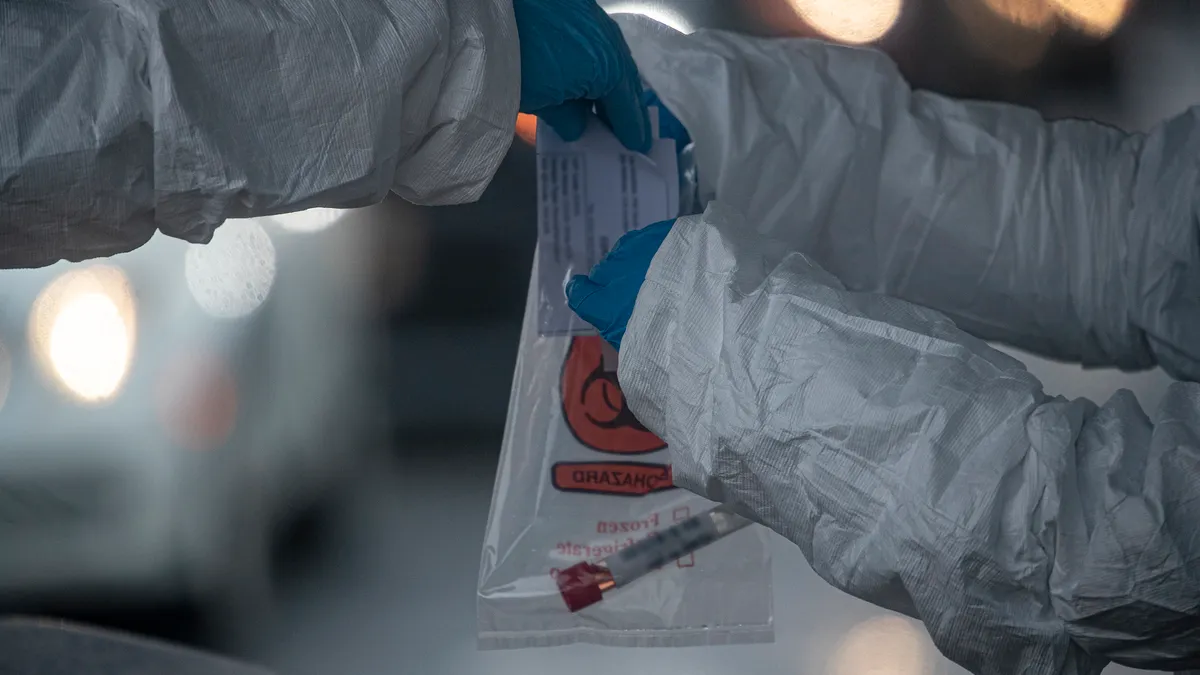
Laboratories have identified commercially available test kits and platform-specific consumables as the top two COVID-19 supply chain constraints as they struggle to increase testing capacity.
-
In a survey conducted from Aug. 13 to Sept. 11 and reported Thursday, 76% of labs polled by the Association for Molecular Pathology said they were currently experiencing limited supplies of commercially available testing kits. More than half of respondents were dealing with shortages of platform-specific consumables such as pipette tips.
-
The survey revealed areas of improvement since a poll conducted early in the pandemic, with far fewer respondents reporting shortages of swabs and transport media. Roche’s cobas is the most commonly used platform, followed by Abbott’s RealTime and Hologic's Aptima among commercial testing methods. Survey respondents reported not experiencing significant numbers of false negatives (87%) or false positives (89%).
Dive Insight:
Even as the medtech industry has scaled up availability of coronavirus diagnostics, without enough testing supplies to go around U.S. labs continue to report constraints.
In May, AMP released findings from a survey of laboratories it conducted the previous month. The survey quantified anecdotal reports of shortages that had already emerged, revealing that 87% of laboratories had delayed or decreased testing due to supply chain interruptions or limitations. Since that poll, companies such as Thermo Fisher Scientific, which invested $40 million in a viral transport media plant, have acted to meet surging demand.
The August poll shows the actions have benefited laboratories. In April, 53% of laboratories reported transport media shortages and 60% said swabs were in short supply. By August, less than 30% of the polled laboratories were still struggling to access either material.
AMP noted that the Trump administration in May worked to distribute swabs and viral transport media to states to help them with testing reagent shortages. However, when survey respondents were asked if their laboratory had received VTM or swabs from the federal government, only 20% and 17% of labs respectively indicated that they received these items. "Of those who did receive government-procured supplies, only about 40% felt that these supplies aided their laboratory's ability to maintain or expand testing capacity indicating it wasn't enough support."
Nonetheless, improved availability of swabs and transport media has eased one restriction to the scale up of U.S. testing capacity. Still, almost half of respondents said demand is exceeding their capacity, up from 29% in April. While many labs are working to add capacity, with 56% of groups aiming to process more than 1,000 tests a day, as of last month just 29% of survey respondents could handle more than 1,000 tests a day.
However, the supply chain remains a problem. Most laboratories are experiencing disruptions in the availability of commercially available testing kits and product-specific consumables. Respondents named those two sets of products as the things they need most to maintain testing, ahead of trained technologists, general consumables and testing platforms.
The emergence of commercially available testing kits and product-specific consumables as the top two supply chain hangups follows a shift in the types of test run by laboratories. In April, half of polled laboratories were using commercial testing kits with emergency use authorization. That figure rose to 62% in the August poll, likely reflecting growth in the number of tests with EUAs.
Many respondents continue to use laboratory developed testing procedures with EUA submissions but have run into challenges with FDA. One-third of respondents said it took more than one month to receive an EUA from FDA. A similar proportion said they faced hurdles in the process. Several respondents filed for emergency use authorization in April and were still waiting in August.
Feedback on the EUA process contributed to an AMP recommendation that agencies “ensure that regulatory requirements for clinical laboratories are not duplicative or burdensome, especially during a pandemic.” AMP said keeping CMS in charge of overseeing laboratory developed tests will ensure the U.S. “can rapidly develop and deploy the testing needed during a public health emergency."
AMP's recommendation comes on the heels of FDA's announcement on Wednesday that it will no longer review emergency use authorization submissions for COVID-19 laboratory developed tests. The move follows a shift by HHS in August when it said FDA would no longer require premarket review for LDTs but labs could voluntarily seek approval, clearance or emergency use authorization.
Now, FDA is effectively shutting the door on new submissions as well as those already in the pipeline for review. The American Clinical Laboratory Association in a statement said FDA's decision creates "unnecessary confusion" and argued that the agency should continue to allow labs to voluntarily submit EUAs.