Dive Brief:
-
Health insurer Cigna has agreed to cover Senseonics’ Eversense implantable continuous glucose monitoring system, giving it access to an additional 17 million covered lives.
-
Cigna was one of three big payer coverage gaps, in addition to Anthem and UnitedHealthcare, identified by Senseonics' CEO late last year.
-
Shares in Senseonics closed up 24% Tuesday on the news. The Connecticut-based insurer sells Medicare Advantage plans in 17 states and Washington, D.C., shifting the geographies where Senseonics has coverage.
Dive Insight:
Senseonics went into 2019 aiming to end the year with 100 million covered lives. In the end, the implantable CGM specialist eased past that target as decisions by organizations including Blue Cross Blue Shield, Humana and Medicare left it with more than 150 million covered lives. The list of payers covering Eversense also includes Aetna, Tricare and Molina Healthcare.
The coverage decisions gave Senseonics a platform from which to grow revenue of its Eversense CGM, which underperformed expectations over the first nine months of 2019, but still left it with sizable gaps in payer support.
Talking to investors in November, Senseonics CEO Tim Goodnow, a former executive in Abbott's diabetes division, identified Anthem, Cigna and UnitedHealthcare as the three largest commercial payers the company still needed to win over.
Cigna began covering Eversense CGM Feb. 15, giving Senseonics access to 17 million more lives and eliminating one of Goodnow’s outstanding targets.
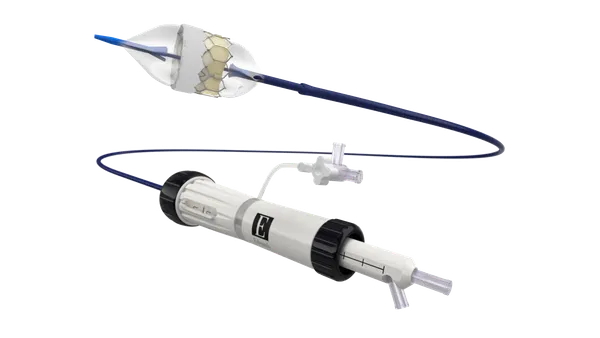
The Cigna policy says Eversense, a continuous glucose monitoring system with an implantable interstitial glucose sensor, is considered medically necessary for management of Type 1 or Type 2 diabetes in people 18 years old and up who are using multiple daily injections of insulin or a continuous subcutaneous external insulin pump.
Cigna also has coverage policies for CGMs made by Abbott, Dexcom and Medtronic.
Now, Senseonics is aiming to further convince patients and physicians to opt for its implantable CGM. The Germantown, Maryland-based company reduced the size of the sales force working to achieve that goal late last year, framing the restructuring, which entailed the “immediate elimination of approximately 30% of current open and planned headcount,” as a way to focus on regions where it had payer coverage and reduce spending in other geographies.
Goodnow discussed the impact of securing coverage from the remaining three big commercial payers on a third quarter earnings call, describing the anticipated addition of the new covered lives as a trigger for a step up in investment.
“As those covered lives come on, I would anticipate that we would have further incremental resources and do more broad-based coverage,” Goodnow said.
Senseonics shared news of Cigna’s decision one week after it entered into a partnership with Companion Medical, the manufacturer of the InPen injection management system. The partnership will see glucose data from Eversense CGM integrated into InPen to inform insulin delivery.