Dive Brief:
- A small, retrospective study suggests high intensity focused ultrasound (HIFU) ablation is a viable alternative to radical treatment in men with localized prostate cancer.
- The study, published in The Journal of Urology, found only 9% of 100 patients treated with SonaCare Medical's Sonablate 500 or EDAP TMS' Ablatherm needed surgery or radiation over the subsequent two years.
- While noting the limitations of the study of procedures performed at two U.S. facilities by three surgeons, the researchers see the data as evidence that HIFU is safe and provides "adequate short-term cancer control." Larger, prospective and controlled studies are needed to more definitively show how well the technology works.
Dive Insight:
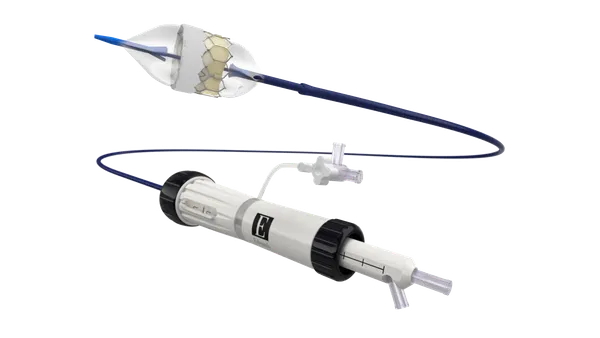
The start of the U.S. market for HIFU ablation of prostate tissue dates back to late 2015, when FDA cleared Sonablate and Ablatherm within weeks of each other. Profound Medical joined the field last year when FDA cleared TULSA-PRO, which the company sells alongside a non-cancer HIFU device it acquired from Philips.
Advocates of HIFU ablation tout it as a way to treat prostate cancer in an outpatient procedure without exposing patients to the risks of surgery and radiation, which are associated with negative quality of life outcomes including urinary incontinence and impotence.
To understand how the technology is performing in the real world, researchers at the University of Southern California reviewed the outcomes of 100 men who underwent hemigland HIFU for prostate cancer. The primary endpoint was treatment failure, defined as the presence of medium-grade tumors or metastases, the need for radical treatment (which in some cases is considered removal of the prostate) or systemic therapy or death due to prostate cancer.
Two years after HIFU treatment, 27% of participants had experienced one or more of the negative outcomes featured in the definition of treatment failure, 24% of men had clinically significant prostate cancer and 9% had required radical treatment.
Men who were classed as low-risk, at worst, at baseline fared best. In that cohort, 16% of people had clinically significant prostate cancer after two years, compared to 37% in the highest-risk group.
The repeatability of HIFU enabled surgeons to spare some men from the need to undergo surgery or radiation even after their conditions worsened following the initial treatment. The research showed 10% of men in the trial underwent another HIFU procedure in the two-year period analyzed by the researchers.
Patient-reported outcomes suggest HIFU has no significant effect on sexual function and the researchers saw no new onset urinary incontinence, validating the use of the procedure as a way to preserve quality of life.
The results are in line with the findings of a study and systematic review of patients treated outside of the U.S., where there is a longer history of using HIFU in prostate cancer. However, the limitations of the U.S. study make it impossible to draw concrete conclusions.